WHAT IS ANGINA? IS ANGINA DANGEROUS? CAUSES, SYMPTOMS, TYPES OF ANGINA, AIS ANGINA HEREDITARY? UNSTABLE ANGINA, DIAGNOSIS, TREATMENT
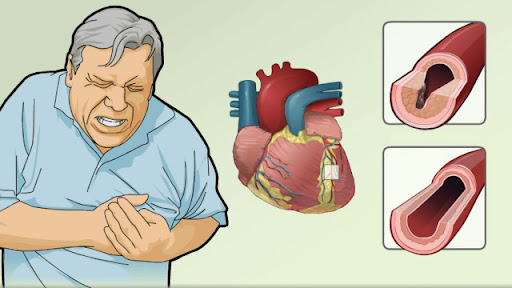
Angina is a chest pain or discomfort that occurs when your heart muscle does not get enough oxygen. It may feel like pressure or squeezing in your chest. Discomfort may also be on your shoulders, arms, neck, jaw or back.
- WHAT IS ANGINA
- MAIN CAUSES
- IS ANGINA HEART ATTACK? /WHAT HEART ATTACK?
- CAN ANGINA GO AWAY?
- TYPES
- SYMPTOMS
- DIAGNOSIS
- TREATMENT
WHAT IS ANGINA?
Angina is a tightness, pressure, strain or pain in the chest. This occurs when the heart muscle area receives less blood oxygen than normal.
Angina is not a disease, it is a symptom. It is usually caused by ischemia, when one or more coronary arteries constrict or become blocked. It is often a symptom of coronary heart disease (CHD).
Alone, angina is not fatal, but it is similar to the symptoms of a heart attack and is a sign of heart disease.
If angina occurs accidentally, does not go away, or does not rest or respond to medication, seek medical help.
Is Angina Dangerous?
Angina is a chest pain caused by decreased blood flow to the heart muscle. This is usually not fatal, but is a warning sign that you are at risk for heart attack or threat of life. With treatment and healthy lifestyle changes, it is possible to control angina and reduce the risk of these more serious complications.
Causes Of Angina:
- The blood supply to the heart comes from the coronary arteries that come out of the aorta as soon as they come out of the heart. The coronary arteries run along the surface of the heart and are divided into smaller and smaller blood vessels, which support each muscle cell of the heart. The most common reason patients complain of angina is coronary arteries caused by atherosclerotic heart disease (ASHD).
- Cholesterol plaque gradually forms on the inner layer of the coronary artery, reducing its diameter and reducing the amount of blood flowing after the blockage. When the heart is asked to work harder and pump harder and faster, not enough oxygen is provided beyond the barrier to meet the energy demand of the myocardium and this can lead to angina symptoms.
- When a plaque ruptures, a blood clot forms, which completely blocks the coronary artery and blocks blood flow to the part of the heart muscle that supplies the artery. This is called a heart attack or myocardial infarction and is a medical emergency. The heart muscle that loses blood supply dies and is replaced by scar tissue that does not contract. This can reduce the pumping capacity of the heart as before. In addition, the heart muscle that loses blood supply can become irritated and lead to heart rhythm disturbances such as ventricular fibrillation or ventricular flutter, which can lead to sudden cardiac death.
- Unstable angina occurs when there is a severe restriction on the blood supply to the heart due to blood clots.
- Over the years, fat deposits or atheromas form in the arteries. As a result, the arteries constrict and limit the amount of blood reaching the heart.
- If these fat deposits burst or break, it can interfere with blood flow, which can lead to blood clots. These dilate and block the arteries, causing unstable angina symptoms.
- AHA Note This blood clot is partially dissolved and re-formed. Symptoms of Unstable Angina Each time a blood clot restricts blood flow in the artery.
- Every heartbeat sends blood not only to the body, but also to itself, there are many different systems in the body and inside the heart that normally work to provide oxygen to the heart muscle. Angina can occur if any of them, individually or in combination, fails to function adequately. Examples include the following:
Angina in the chest includes the following sensations:
Indiges
Stress
Inertia
Tight
Inflammation or pain in the chest, usually starting from the back of the breast bone
The pain often radiates to the neck, jaw, arms, shoulders, throat, back or teeth.
Other possible features:
Indigestion
Stomach irritation
Weakness
Strive, cramps
Nausea comes on, vomiting
Patting
Difficulty in breathing
The duration of these symptoms depends on the type of angina.
Anyone experiencing severe or persistent chest pain should call 911 or seek emergency care.
Symptoms in women:
In any case, angina can arise from CHD or MVD.
MVD affects women more than men, and as a result, the American Heart Association (AHA) explains, women can experience a wide variety of symptoms, including angina.
As well as chest pain, which can be exacerbated, a woman with angina may experience:
Nausea and vomiting
Abdominal pain
Fatigue
Difficulty in breathing
AHA women were asked to seek help for symptoms of heart disease. They emphasize that heart disease is the leading cause of death.
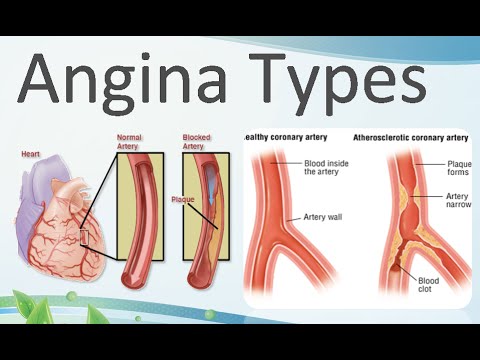
Types Of Angina:
There are several types of angina, including:
1-Constant / Stable angina
Constant angina occurs when the heart is working more than normal - for example, during exercise. It usually lasts about 5 minutes.
It has a simple pattern and a person can experience it for months or even years. Rest or medications often relieve symptoms.
2-Unstable Angina:
Unstable angina does not follow a normal pattern and usually occurs at rest. It mostly occurs as a result of atherosclerosis, which is a barrier that prevents blood from reaching the heart.
The pain lasts for more than 5 minutes and worsens over time. Rest and medication alone may not improve symptoms.
Persistent angina indicates a risk of heart attack. Anyone with unexpected angina should seek emergency care.
3-Microvascular angina:
Microvascular angina can occur with coronary microvascular disease (MVD). It affects the smallest coronary arteries.
As well as chest pain, a person may experience:
Fatigue and low energy
Sleep problems
Difficulty in breathing
Microvascular angina is more common than stable angina. This is often more than 10 minutes and sometimes more than 30 minutes.
4-Variant angina:
Variant angina is rare. Doctors sometimes call it prinzmetal angina and it develops when the body is at rest, often at midnight or in the morning.
It occurs when there is spam in the coronary arteries. Possible triggers include cold, stress, medication, smoking or cocaine use.
It is a chronic condition, but medications can help manage it.
Is Angina Hereditary?
Heart disease runs in families, so if you have a first-degree relative (mother, father, brother or sister) with a history of heart disease or angina, the risk of developing angina increases.
Diagnosis:
To diagnose angina, your doctor will start by doing a physical exam and asking about your symptoms. You will also be asked about any risk factors, including whether you have a family history of heart disease.
There are several tests your doctor can do to determine if you have angina:
1-Electrocardiogram (ECG or EKG):
Every beat in your heart is triggered by an electrical impulse generated by specific cells in your heart. An electrocardiogram records these electrical signals as they travel through your heart. Your doctor may look at patterns between these heartbeats to find out if your blood flow to your heart has slowed or interrupted or if you have had a heart attack.
2-Stress test:
Sometimes it is easier to diagnose angina when your heart is working hard. During a stress test, you exercise by walking on a treadmill or pedaling a stationary bicycle. Monitor your blood pressure and ECG readings while you exercise. Other tests can be done at the same time as the stress test. If you are unable to exercise, you may be given medications that make your heart more difficult to exercise, and then undergo an imaging test.
3-Echocardiogram:
The echocardiogram uses sound waves to create heart images. Your doctor may use these images to diagnose angina-related problems, such as damage to the heart muscle due to poor blood flow. An echocardiogram can be given during a stress test and can show if there are areas in your heart where there is not enough blood.
4-Nuclear pressure test:
The nuclear stress test can help measure blood flow to your heart muscle during rest and during tension. This is similar to a normal pressure test, but during a nuclear stress test, a radioactive substance is injected into your bloodstream.
This substance mixes with your blood and travels to your heart. A special scanner that detects radioactive material in your heart - shows how the substance moves with the blood in your heart muscle. As you can see in the pictures the blood flow to any part of your heart is low because the radioactive material is not so much.
5-Chest X-ray:
This test takes pictures of your heart and lungs. This is to look for other conditions that describe your symptoms and to see if your heart is expanding.
Blood test. If your heart is damaged by a heart attack, some heart enzymes are slowly released into your bloodstream. Your blood samples can be tested for the presence of these enzymes.
6-Coronary angiography:
Coronary angiography uses X-ray imaging to examine the inside of your heart blood vessels. It is part of a common group of processes called cardiac catheterization.
During coronary angiography, a type of pigment that is visible through an X-ray machine is injected into your coronary arteries. The X-ray machine rapidly takes an array of images (angiogram), which gives a detailed look inside your blood vessels.
7-Cardiac computed tomography (CT) scan:
On a cardiac CT scan, you lie on a table inside a donut-shaped machine. An X-ray tube inside the machine moves around your body and collects images of your heart and chest, which can show if your heart is narrowing or if your heart is dilated.
8-Cardiac MRI:
In a cardiac MRI, you lie on a table inside a long, tube-like machine that produces detailed images of the structure of your heart and its blood vessels.
Other conditions can also cause chest pain, including:
Pulmonary embolism (pulmonary artery obstruction)
Aortic dissection (rupture of the main artery)
Lung infection
Aortic stenosis (narrowing of the aortic valve of the heart)
Hypertrophic cardiomyopathy (heart muscle disease)
Pericarditis (inflammation of the tissues surrounding the heart)
Terrible attack.
Angina Is Heart Attack / What Is Heart Attack?
Angina:
Is a term used to describe chest pain that occurs without adequate blood flow to the heart. When the heart does not receive enough blood, your body sends out warning signals that you are at risk of heart damage. Angina is a specific type of pain that you experience when you have a heart problem.
Heart attack:
On the other hand, it occurs when the contraction is severe or obstructed, causing actual damage to the heart muscle. In other words, heart attack is a real medical condition and a symptom of angina.
- [Here's another way to look at it: When your heart is not getting enough blood, you get angina, and when your heart is actually damaged due to blood loss, heart attack occurs.]
Treatment is to reduce pain, stop symptoms and prevent or reduce the risk of heart attack. A physician may prescribe medications, lifestyle changes, a surgical procedure, or a combination.
1-Lifestyle changes
The following strategies may help:
- Quit smoking
- Weight management
- Checking cholesterol levels regularly
- Rest when needed
- Exercise regularly
- Learning to manage or prevent stress
- Eat a diet high in fruits, vegetables, whole grains, low - fat, or not - dairy products, and lean sources of protein
2-Drugs / Medications:
Doctors often prescribe nitrates such as nitroglycerin for angina. Nitrates prevent or reduce the severity of angina by relaxing and dilating blood vessels.
Other options include:
- Beta blocker
- Calcium channel blockers
- Angiotensin covers enzyme inhibitors
- Anti-platelet drugs
- Anticoagulant
- Statins, which are cholesterol-lowering drugs
Medications that manage high blood pressure can help manage angina. These include lowering blood pressure and cholesterol levels, lowering heart rate, relaxing blood vessels, reducing stress on the heart and preventing blood clots.
Options other than surgery:
If medications do not help, other treatments
Improved External Counterpulsation Therapy:
This involves wearing a device such as a blood pressure cuff to improve the flow of oxygen to the heart.
Spinal Stimulators:
These prevent the sensation of pain but do not directly improve heart health.
Transmyocardial laser therapy:
It stimulates the growth of new blood vessels or increases blood flow to the heart.
Surgical procedures
In some cases, a procedure is required. A heart specialist may recommend angioplasty, perhaps with a stent implant.
Alternatively, cardiologists may recommend coronary artery bypass grafting, in which a surgeon uses a healthy artery or vein from another part of the body to bypass the narrow arteries in the heart.
Homeopathic Medicines For Heart Diseases:
Aurum Metallicum:
Heart failure after valvular injuries. The heater feels loose when running. The turbulent reflex comes on as soon as the heartbeat seems to have stopped for two or three seconds, immediately sinking into the epigastrium. Heart suppression. The pulse is fast, weak and irregular. High blood pressure.
Digitalis purpurea:
It is an excellent remedy for heart failure with irregular heartbeat. The feeling that the heart stops beating while shaking, the breath must be kept intact. The pulse is full, irregular, very slow and weak, intermittent every third, fifth or seventh beat. Weak heart. Minimal movement beats violently. Frequent piercings in the heart.
Strophanthus:
It is best for heart failure with swelling of the legs. Heart function is weak, rapid, and irregular due to muscle weakness and deficiency. Pulse becoming faster, slower, weaker, short irregular.
Cretaceous:
It is a tonic for the heart. The heart muscle feels loose and worn out. Heart weakness with epilepsy, stitches and insomnia. Severe shortness of breath with minimal effort without much increase in pulse. The heart was wide, at first the tone was weak. Inefficient valve, valvular murmur.
Cardus Marianus:
Effective for heart failure with liver complaints. Traumatic pressure and stitches in the heart area, pressure on deep breathing.
Naja Tripudian:
Heart failure with weakness and valve disorders. Beat visible. Heart damage after infectious diseases.
Lauroceracus:
It is best for heart failure with pain in the heart area. There is tightness and palpitations in the heart. Pulse can be weak, variable, slow or irregular. , maintained, involuntarily beaten and suppressed with shortness of breath and convulsions.
ALWAYS USE HOMOEOPATHY MEDICINES WITH DOCTOR'S ADVISE AND COMPLETE SYMPTOMS.FOR MORE HEALTH RELATED INFORMATIONS VISIT CHANNEL;













3 Comments
👍👍👌👌👌first time atni detail zbrdst sunni thnkxxx dr Tayyiba bhoot bhoot infrmative blog but so hardworking and great work. Apka field apko promote kry bcz u did excellent work 4 it homopathy field.bst lukkk Dr shiba ❤❤❤❤💖💖💕💕💕
ReplyDeleteBoot muskal work medical article likhna bcz restricted ho jata ha.bhooot appreciated hoo ap..👌👌👌👍👍👍👍❤❤💕💖
ReplyDeleteWaqas MBA.UAE
ReplyDeletedil se thnks mery dada ko prblm ha.bhoot infrmative blogs👌👌👌👍👍👍👏👏👏